Table of Contents
- What Is Retinoblastoma?
- The Genetics Behind Retinoblastoma
- Understanding Genetic Risk Factors
- Key Genetic Risk Factors
- Hereditary vs Non-Hereditary Retinoblastoma
- How Genetic Testing Can Help
- Preventive Measures and Early Detection
- Surveillance for High-Risk Children
- Support and Resources for Families
- Conclusion
- FAQs
Retinoblastoma is a rare but life-threatening eye cancer that primarily affects young children, typically those under the age of five. Since the most common malignant tumor of the eye in childhood is Retinoblastoma, understanding its genetic risk factors is essential for early recognition, timely intervention, and better clinical outcomes. By exploring the causes of Retinoblastoma, hereditary factors, genetic mutations, and avenues for prevention through this insightful blog, parents can be empowered to take an active role in safeguarding their child’s vision and health.
What Is Retinoblastoma?
Retinoblastoma is a malignant tumor that develops in the retina, the thin layer of tissue at the back of the eyeball responsible for sensing light and transmitting images to the brain. Key facts include:
Key Insights
- Prevalence: About 1 in 15,000 to 20,000 live births globally.
- Age: Most diagnoses occur before the age of five.
- Laterality: Can affect one eye (unilateral) or both eyes (bilateral). Bilateral cases are more likely due to genetic mutations.
Symptoms
- Leukocoria (white reflection in the pupil)
- Strabismus (crossed eyes)
- Poor vision or eye redness/swelling
Comparison of Unilateral vs. Bilateral Retinoblastoma
| Feature | Unilateral (One Eye) | Bilateral (Both Eyes) |
| Incidence | ~60% of cases | ~40% of cases |
| Age at diagnosis | 18–36 months | Often <12 months |
| Genetic link | Less likely | Highly likely |
Early detection and prompt treatment of retinoblastoma are critical for saving vision, the eye, and preventing metastasis (spread to other parts of the body such as the brain or bones).
The Genetics Behind Retinoblastoma
Genetics play a pivotal role in retinoblastoma. The disease most often results from mutations in the RB1 gene, a tumor suppressor gene located on chromosome 13. Its main function is to regulate the cell cycle and prevent cells from growing uncontrollably.
RB1 Gene Mutation:
- Both copies of the RB1 gene must be altered for a cell to become cancerous.
- Germline (inherited) mutations mean one defective copy is present in all cells at birth, increasing risk.
- Somatic (acquired) mutations occur only in retinal cells and are not inherited.
Mutation Facts:
- Children with a germline mutation in RB1 have a 40% chance of developing retinoblastoma.
- About 10‒20% of children with retinoblastoma have no family history — these are de novo mutations.
- Germline mutations increase the risk of other cancers later in life (e.g., osteosarcoma).
Did you know?
The discovery of RB1 was pivotal in cancer genetics, marking the first identification of a tumor suppressor gene.
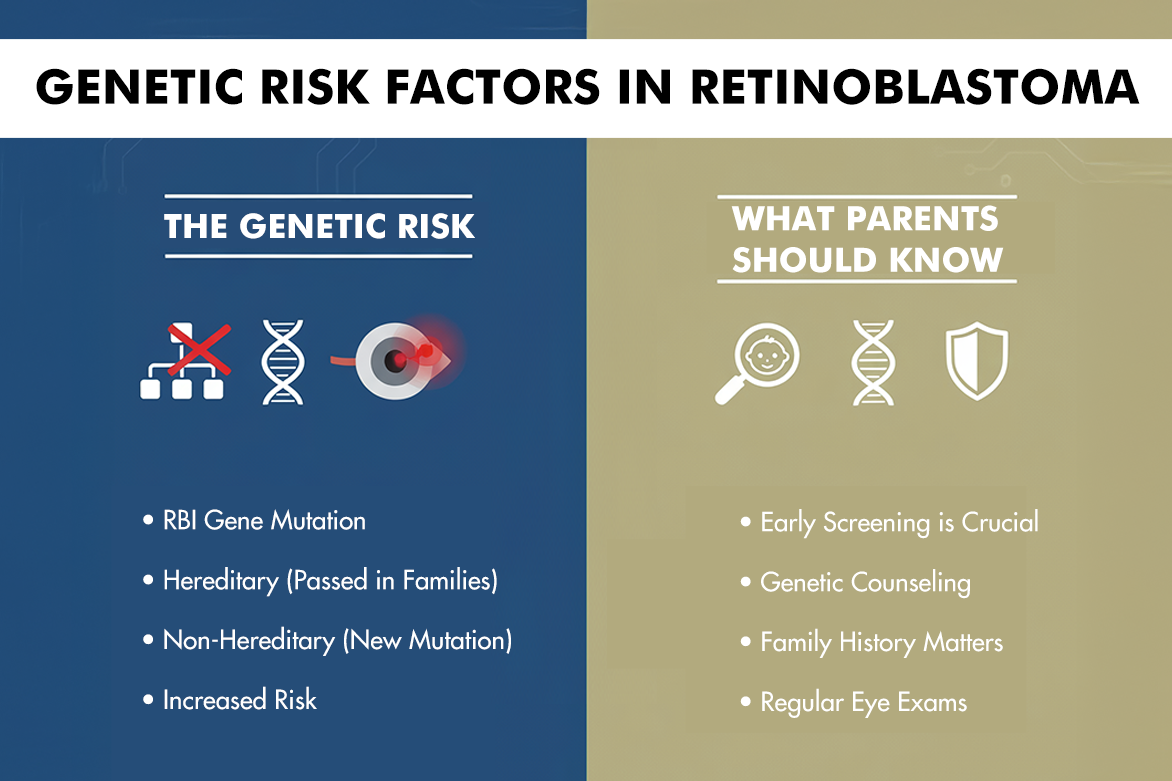
Understanding Genetic Risk Factors
The risk of retinoblastoma is strongly influenced by genetic inheritance:
- If a parent carries an RB1 mutation, each child has a 50% chance of inheriting it.
- Not all children who inherit the mutation develop cancer, but their risk is significantly elevated.
- Families with a history of retinoblastoma benefit greatly from genetic counseling and regular screening.
Key genetic risk factors:
Inherited (Germline) Mutation:
- Found in every cell of the body, including reproductive cells.
- Can be passed to future generations.
- Responsible for nearly all bilateral cases.
Sporadic (Somatic) Mutations:
- Occur only in retinal cells.
- Not inherited or passed on to children.
- Most unilateral cases fall into this category.
Fact Box
- Approximately 60% of retinoblastoma cases are non-hereditary (somatic) and confined to one eye.
- About 40% are hereditary (germline), with a higher likelihood of affecting both eyes and being present at a younger age.
Hereditary vs Non-Hereditary Retinoblastoma
A clear understanding of the distinction between hereditary and non-hereditary retinoblastoma shapes both screening and management approaches.
| Feature | Hereditary Retinoblastoma | Non-Hereditary Retinoblastoma |
| Cause | Germline RB1 mutation | Somatic RB1 mutation |
| Laterality | Often bilateral | Usually unilateral |
| Family history | Frequently present | Usually absent |
| Sibling risk | Increased | Not elevated |
| Age at diagnosis | Earlier (<1 year) | Later (1–3 years) |
| Other cancer risk | Higher (second malignancies) | Not increased |
How Genetic Testing Can Help
Genetic testing utilizes advanced techniques to detect RB1 gene mutations. It enables:
- Identification of at-risk family members before symptoms appear
- Precision diagnosis, guiding treatment decisions
- Reduced need for invasive eye exams under anesthesia in unaffected siblings
Benefits of Genetic Testing:
- Allows early screening and surveillance for those who test positive
- Guides reproductive decisions for parents/families
- Reassurance for those who do not carry the mutation
Testing Process:
- Collection of blood or saliva samples
- DNA analysis to identify RB1 gene mutations
- Results counseling to discuss findings and next steps
Limitations to Keep in Mind:
- Not all mutations are detectable with current technology
- Results may impact family dynamics and psychological well-being—support is vital
Preventive Measures and Early Detection
Early detection significantly improves outcomes and can even save lives. Key preventive and surveillance strategies include:
Routine Eye Examinations:
- Frequent, thorough eye exams for children at risk (including those with a family history)
- Use of tools such as fundus photography, ultrasound, and MRI
Monitoring for Warning Signs:
- Leukocoria (white reflection in the pupil—often the first sign noticed in photographs)
- Strabismus or misaligned eyes
- Poor vision or unexplained changes in a child’s eye appearance
Parent Action Checklist:
- Be vigilant for changes in your child’s eye or vision
- Attend all scheduled pediatric eye appointments
- Inform your child’s doctor about any family history of retinoblastoma or eye cancer
Fact: Early diagnosis improves the survival rate of retinoblastoma above 95% in developed countries.
Surveillance for High-Risk Children
Close, lifelong monitoring is essential for children with hereditary risk. Best practices include:
- Regular Eye Exams: Often every few months in infancy and childhood
- Imaging: Use of ultrasound, MRI to detect tumors not visible by standard examination
- Extended Screening: Lifelong monitoring is advised due to increased risk for secondary non-eye tumors
Surveillance Protocol Example
- Newborn to 3 years: Eye exam every 3–4 months
- 3–7 years: Eye exam every 6 months
- After 7 years: Annual exams or as advised by the healthcare team
Support and Resources for Families
Managing retinoblastoma involves both medical and emotional challenges. Families can draw on a range of support services:
- Genetic Counseling: Offers individualized risk assessment, education, and guidance in decision-making
- Support Groups: Local and international groups provide community, shared experiences, and hope
- Healthcare Teams: Pediatric oncologists, ophthalmologists, geneticists, and counselors coordinate comprehensive care
Organizations & Resources:
- Retinoblastoma International: Information and advocacy
- Childhood Eye Cancer Trust: Support and funding for research
- Centre For Sight: Specialized care, world-class treatment, and long-term follow-up
Conclusion
Genetic counseling and testing are foundational in assessing risk for children and families. Regular monitoring, especially for high-risk children, significantly increases the likelihood of successful outcomes. Early detection and timely treatment not only preserve vision but can be lifesaving. Accessible support and resources empower families to navigate the journey with strength and resilience. With continued research and advances in genetic medicine, hope for families facing retinoblastoma grows stronger every day.