Table of Contents
- The Silent Thief of Sight: Understanding Glaucoma
- Why Glaucoma Monitoring Matters?
- How Glaucoma Progresses Over Time
- Identifying Key Risk Factors for Glaucoma Progression
- The Role of Advanced Diagnostic Tools in Monitoring Glaucoma
- Personalized Monitoring: Tailoring Treatment Plans for Individual Patients
- Future Directions in Glaucoma Management and Monitoring
- Conclusion
- FAQs
Glaucoma is an eye condition that can lead to vision loss and blindness by damaging the optic nerve in the back of the eye. Often referred to as the ‘silent thief of sight,’ glaucoma progresses gradually and can be asymptomatic in its early stages. It signifies that early detection and continuous monitoring are essential for preventing significant vision impairment.
Through this comprehensive blog by the Centre For Sight, we will explore the glaucoma disease progression, identify key risk factors of glaucoma, discuss the importance of personalized monitoring, and highlight the latest advancements in diagnostic tools.
The Silent Thief of Sight: Understanding Glaucoma
Glaucoma encompasses several types, including open-angle glaucoma, angle-closure glaucoma, and normal-tension glaucoma. Each type affects the eye differently, but all result in optic nerve damage. This damage is often associated with elevated intraocular pressure (IOP), though normal-tension glaucoma occurs without a significant increase in IOP. In fact, open-angle glaucoma is the most common form, accounting for nearly 90% of all cases worldwide. According to the World Health Organization, glaucoma is the second leading cause of blindness globally, affecting over 76 million people. Alarmingly, it is estimated that nearly half of those living with glaucoma are unaware of their condition, highlighting the importance of widespread screening. The condition can progress silently, causing irreversible damage before noticeable symptoms arise. Therefore, understanding the disease mechanism and recognizing its subtle early signs are critical for effective glaucoma treatment. Early intervention can make a profound difference in slowing vision loss and maintaining quality of life.
Why Glaucoma Monitoring Matters?
Regular monitoring of glaucoma is crucial for protecting vision and overall quality of life. Consistent check-ups help ophthalmologists detect even subtle changes in eye health—often before the patient notices symptoms. Studies reveal that up to 40% of vision can be lost to glaucoma without any warning signs, underscoring the threat of undiagnosed progression. Without regular monitoring, patients risk irreversible vision loss that severely impacts day-to-day living.
Effective monitoring empowers physicians to tailor treatment plans and intervene at the right time, especially since vision lost to glaucoma cannot be restored. Because progression of glaucoma disease can be silent and each patient’s risk varies, individualized monitoring is particularly important for those at higher risk or experiencing rapid changes. Ultimately, timely and attentive monitoring remains the foundation for successful glaucoma care, helping to prevent severe vision impairment and preserve independence.
How Glaucoma Progresses Over Time?
Glaucoma progression happens through a series of stages, each with its own set of challenges. Early on, there are rarely any symptoms, patients often feel their vision is perfectly fine, making this stage easy to overlook without regular exams. As the disease silently advances, early symptoms might include mild peripheral vision loss or difficulty adjusting to dim lighting, though these changes are often missed until they worsen.
In moderate stages, people may notice that their side vision is gradually narrowing, sometimes described as “tunnel vision.” Everyday tasks like driving or moving around unfamiliar spaces can become noticeably harder. In advanced glaucoma, significant vision loss occurs, impacting even central vision in some cases and making daily independence much more challenging.
Because the speed of progression differs for every individual, regular eye exams, including tests for eye pressure, visual field, and optic nerve imaging, are essential at every stage. Catching changes early not only helps protect vision but also allows your ophthalmologist to tailor treatments to your unique needs and slow further damage.
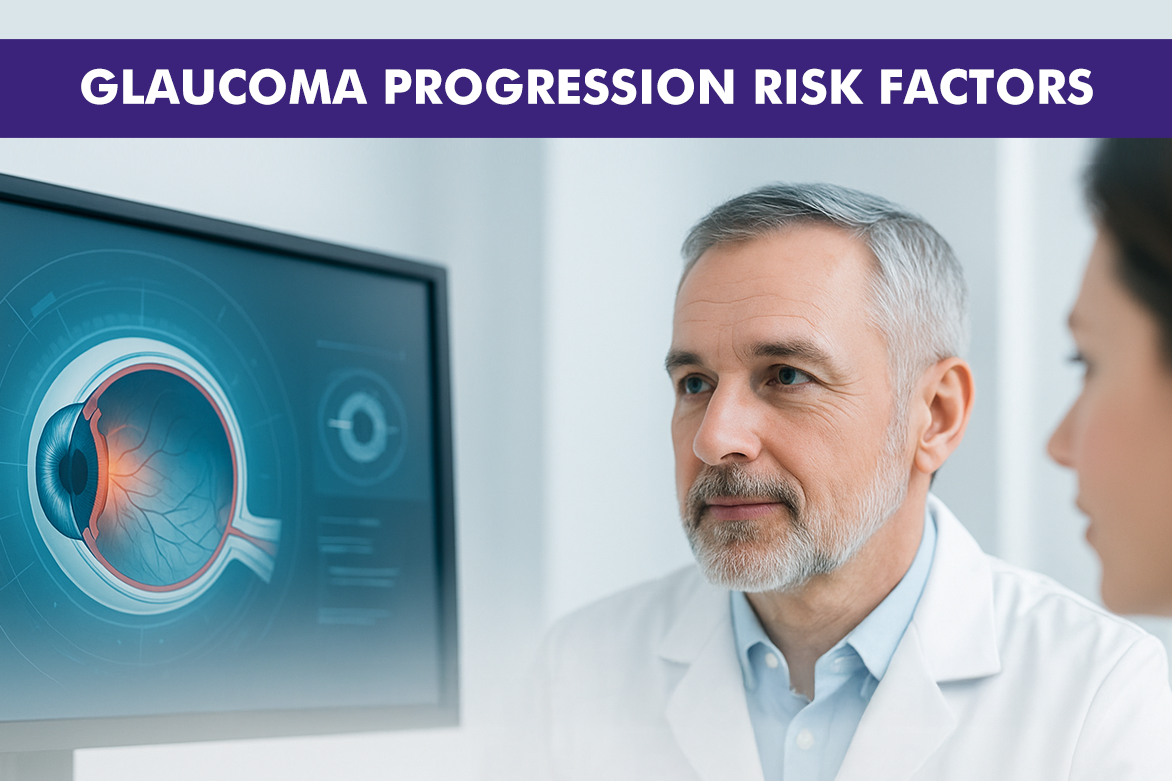
Identifying Key Risk Factors for Glaucoma Progression
- Age: The risk of glaucoma increases significantly after the age of 40. Aging can lead to changes in eye structures, making the optic nerve more vulnerable to damage.
- Family History: Those with a family history of glaucoma are at a higher risk. Genetics can influence eye pressure regulation and optic nerve health.
- Race/Ethnicity: People of African, Hispanic, or Asian descent have a heightened risk. For example, individuals of African descent are more prone to early onset and severe progression.
- High Intraocular Pressure (IOP): Elevated pressure inside the eye is one of the strongest risk factors. High IOP or ocular hypertension can directly damage the optic nerve over time.
- Thin Corneas: A thinner-than-average cornea can underestimate eye pressure in regular tests and may itself indicate greater optic nerve susceptibility.
- Medical Conditions: Diabetes, hypertension, and certain heart conditions can increase the risk. These conditions may affect blood flow to the optic nerve or complicate eye health overall.
- Other Factors: Prolonged use of corticosteroid medications and severe nearsightedness can also elevate glaucoma risk due to their effects on eye pressure and structure.
Recognizing these risk factors of glaucoma helps identify individuals who benefit from more frequent monitoring and early intervention, leading to better outcomes and improved vision preservation.
The Role of Advanced Diagnostic Tools in Monitoring Glaucoma
Advancements in diagnostic tools have significantly improved glaucoma management by identifying the cause of glaucoma progression. Technologies like optical coherence tomography (OCT), visual field analyzers, and retinal nerve fiber layer (RNFL) imaging provide detailed insights into the structure and function of the optic nerve. These tools allow for more precise measurements and can detect changes earlier than traditional methods. This precision is key to tailoring treatment plans and ensuring timely interventions to slow the progression of glaucoma. Many of these technologies also make follow-up visits quicker, more comfortable, and less invasive for patients. As further innovations emerge, early detection and management of glaucoma will continue to become even more effective, helping to preserve vision in more individuals worldwide.
Personalized Monitoring: Tailoring Treatment Plans for Individual Patients
Personalized monitoring involves creating individualized care plans based on a patient’s specific risk factors, disease progression, and response to treatment. This approach ensures that each patient receives the most effective interventions tailored to their unique needs. By utilizing advanced diagnostic tools and considering patient-specific factors, ophthalmologists can develop customized monitoring schedules and treatment strategies that optimize outcomes and preserve vision. Personalized monitoring also helps ensure that changes are detected and addressed early, preventing unnecessary vision loss. It empowers patients to be more engaged in their own care, encourages regular follow-ups, and builds a strong doctor-patient partnership for better long-term eye health.
Future Directions in Glaucoma Management and Monitoring
The future of glaucoma management lies in continued advancements in diagnostic technologies, improved understanding of the disease mechanisms, and the development of novel therapies. Gene therapy, neuroprotective agents, and minimally invasive surgical techniques are among the promising areas of research.
Additionally, artificial intelligence (AI) and machine learning are being explored to enhance diagnostic accuracy and predict disease progression. These innovations easily track how quickly does glaucoma progression happen as well as hold the potential to revolutionize glaucoma care and improve patient outcomes.
Conclusion
Understanding the progression of glaucoma and the importance of personalized monitoring is crucial for effective management of this sight-threatening condition. By identifying key risk factors and utilizing advanced diagnostic tools, ophthalmologists can tailor treatment plans to individual needs, ensuring the best possible outcomes.