Summary: Retinal detachment requires urgent attention. Early detection, awareness of risk factors, and timely retinal detachment surgery or treatment by a specialist can preserve vision and prevent permanent blindness.
|
Key Takeaways:
|
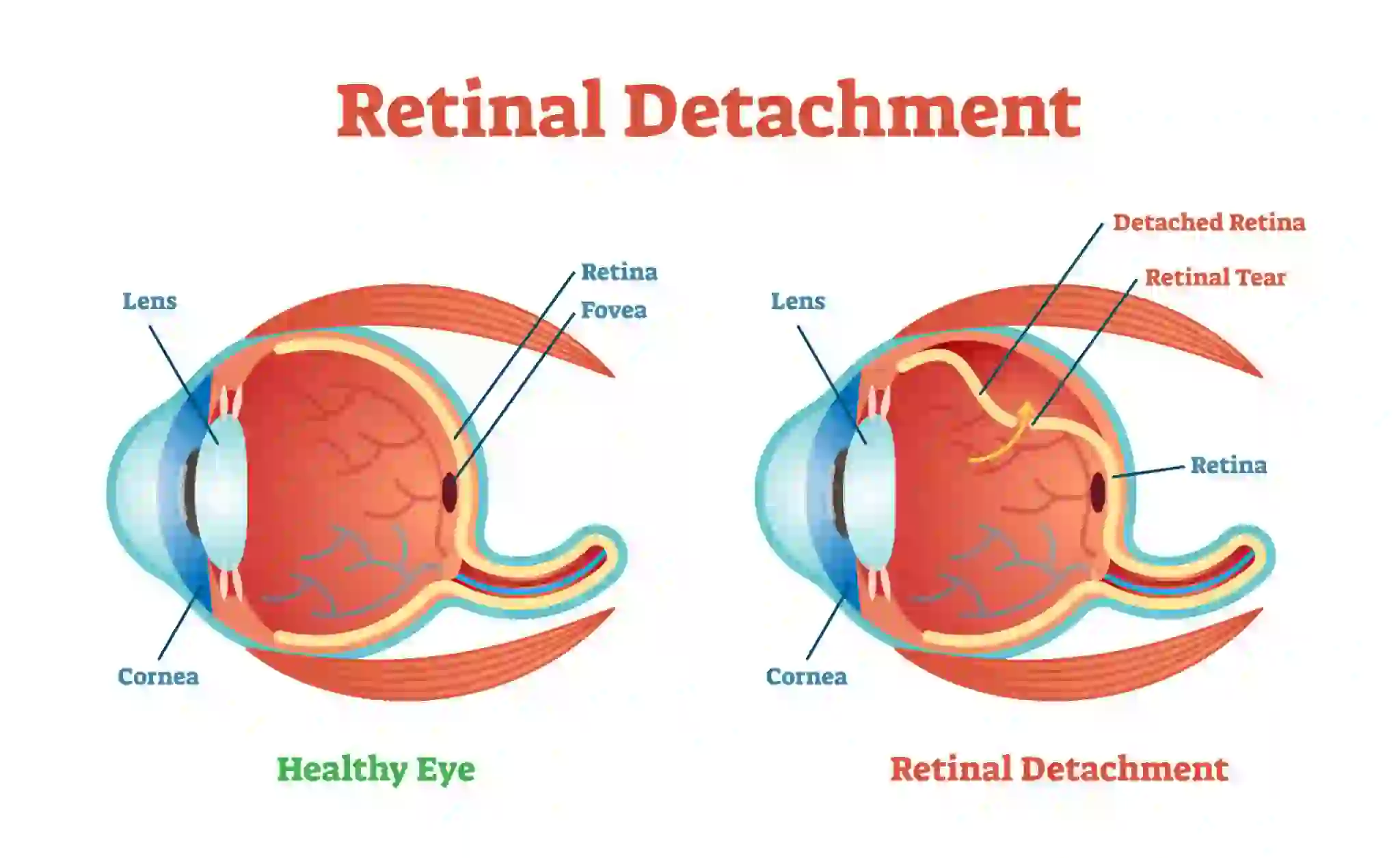
Retinal detachment is a serious eye condition where the retina, the light-sensitive layer at the back of the eye, separates from its underlying tissue. If left untreated, it can lead to permanent vision loss. Consulting a retinal detachment specialist at the first signs can save your vision.
What Is Retinal Detachment?
Retinal detachment happens when the retina – the light-sensitive layer at the back of the eye – separates from the layer that provides it with oxygen and nutrients. This disconnection can stop the retina from functioning, leading to serious vision impairment.
There are three major types:
- Rhegmatogenous: Caused by a tear or hole that allows fluid to seep under and lift the retina.
- Tractional: When scar tissue pulls the retina away from the back of the eye.
- Exudative: Fluid collects under the retina without a tear, often due to inflammation, injury, or underlying disease.
Common Symptoms of Retinal Detachment
- Sudden Floaters or Spots: Tiny dark specks or strings appear in your vision due to debris in the vitreous.
- Flashes of Light (Photopsia): Pulling or irritating the retina causes brief flashes, particularly in peripheral vision.
- Blurred or Distorted Vision: As the retina starts to separate, objects may appear wavy or indistinct.
- Shadow or Curtain Over Vision: A dark curtain-like effect may cover part of your visual field, signalling severe detachment.
These are the main signs of retinal detachment that should prompt immediate medical attention.
Understanding the Main Retinal Detachment Causes
Understanding retinal detachment causes helps in prevention. The types of retinal detachment include:
- Rhegmatogenous Detachment: Caused by a tear or hole in the retina, allowing fluid to seep underneath.
- Tractional Detachment: Occurs when scar tissue pulls the retina away from the eye wall.
- Exudative Detachment: Fluid accumulates beneath the retina without a tear or break.
Risk factors include ageing, high myopia, previous eye surgeries, and a family history of retinal disorders.
Emergency Response: What to Do If You Suspect Retinal Detachment
Think you’re experiencing a detachment? Here’s what to do:
- Contact an ophthalmologist or eye hospital immediately
- Do not rub your eyes – it can worsen the situation
- Keep your head elevated, especially if advised by a doctor
- Avoid self-treatment – this is not something eye drops can fix
Remember: Retinal detachment is not a wait-and-see condition. Fast action can make all the difference.
Available Retinal Detachment Treatment Options
When it comes to retinal detachment treatment, surgery is typically the only way forward. Treatment depends on the type and extent of the detachment. Common procedures include:
- Laser Photocoagulation: A precise laser seals tears
- Cryopexy: Freezing the area to scar it and secure the retina
- Pneumatic Retinopexy: A gas bubble pushes the retina back before sealing
- Scleral Buckling: A silicone band gently presses the eye to support the retina
- Vitrectomy: The vitreous gel is removed and replaced with a bubble or oil to reattach the retina
Each retinal detachment treatment plan is personalised, depending on your condition, lifestyle, and urgency.
Healing After Retinal Detachment Surgery
Recovering from retinal detachment surgery can be demanding, but it’s crucial to follow the aftercare plan meticulously:
- Use prescribed medications, usually antibiotic and anti-inflammatory eye drops
- Limit physical activity – no bending, lifting, or straining
- Follow positioning instructions, especially for gas bubble procedures
- Avoid flying if a gas bubble is in your eye
- Attend follow-up visits to ensure proper healing
Some people notice improved vision within weeks, while others take months to regain clarity. Either way, patience and discipline are key.
Retinal Detachment Prevention: Can It Be Avoided?
Although it isn’t always preventable, you can significantly reduce your risk with some proactive steps. Here’s how retinal detachment prevention works:
- Get regular eye exams, especially if you’re nearsighted or over 40
- Protect your eyes during contact sports or high-risk work
- Control chronic conditions like high blood pressure and diabetes
- Stay alert to retinal detachment symptoms and seek care immediately
- If you’ve had eye surgery, follow your post-op instructions carefully
Retinal detachment prevention is about vigilance and lifestyle. The earlier an issue is caught, the better your visual outcome.
Protecting Your Vision, Preserving Your Life
Yes, retinal detachment can be frightening, but it doesn’t have to mean blindness. With quick diagnosis and the right retinal detachment treatment, most people maintain functional vision. If you ever see flashes, floaters, or shadows in your field of vision, don’t ignore them. Act fast. Your future self will thank you.
FAQs
How long before retinal detachment causes blindness?
Vision can deteriorate within hours to days if untreated. Immediate medical attention is crucial to prevent permanent blindness.
What does retinal detachment look like?
It may appear as a shadow, curtain, or dark area in your vision, often accompanied by flashes or floaters.
What are the signs and symptoms of retinal detachment?
Common signs include sudden floaters, flashes of light, blurred or distorted vision, and a shadow or curtain over part of the visual field.
What is the most common cause of retinal detachment?
The most common cause is a tear or hole in the retina (rhegmatogenous detachment), allowing fluid to seep underneath.
Can one get a detached retina again after treatment?
Yes, it’s possible, especially if you’re at risk (e.g., nearsighted, previous detachment).
Is surgery always necessary for retinal detachment?
Yes, in most cases, surgery is needed to reattach the retina.
Are there any complications or risks associated with retinal detachment surgery?
Yes, risks include infection, bleeding, cataracts, and in rare cases, vision loss.
What is the long-term outlook for someone who has experienced retinal detachment?
With timely treatment, many regain useful vision, but long-term follow-up is crucial.
Is retinal detachment hereditary?
It can have genetic factors, but it’s mostly due to aging or trauma rather than direct heredity.
Can retinal detachment happen again after surgery?
Yes, especially if you’re highly nearsighted or have had a previous detachment. Regular checkups are crucial.
Is surgery always necessary for retinal detachment?
In nearly all cases, yes. Delaying surgery could result in irreversible vision loss.
Are there any complications after surgery?
Risks include infection, cataracts, bleeding, or scar tissue. Your surgeon will guide you on what to expect.
What’s the long-term outlook?
Many regain functional vision, especially with early treatment. Some may experience minor vision distortions.
Is retinal detachment hereditary? Not always, but a family history increases your risk. Combine that with myopia or trauma, and your risk rises.